[av_section min_height=” min_height_px=’500px’ padding=’large’ shadow=’no-border-styling’ bottom_border=’no-border-styling’ bottom_border_diagonal_color=’#333333′ bottom_border_diagonal_direction=” bottom_border_style=” id=” color=’main_color’ custom_bg=’#403393′ src=’https://handbiolab.com/wp-content/uploads/2017/07/sub-banner.jpg’ attachment=’562′ attachment_size=’full’ attach=’parallax’ position=’top right’ repeat=’no-repeat’ video=” video_ratio=’16:9′ overlay_opacity=’0.5′ overlay_color=” overlay_pattern=” overlay_custom_pattern=” av_element_hidden_in_editor=’0′ av_uid=’av-v8xkp’]
[av_heading heading=’Clinical Discussions’ tag=’h1′ style=’blockquote modern-quote modern-centered’ size=” subheading_active=” subheading_size=’15’ padding=’10’ color=’custom-color-heading’ custom_font=’#ffffff’ admin_preview_bg=” av_uid=’av-t39a1′]
Device Solutions for Difficult Problems
[/av_heading]
[/av_section]
[av_heading heading=’Carpal Tunnel Pressure – Our Thoughts on Its Surprising Dynamic Behavior’ tag=’h2′ link=” link_target=” style=” size=” subheading_active=” subheading_size=’15’ margin=” padding=’10’ color=’custom-color-heading’ custom_font=’#403393′ custom_class=” id=” admin_preview_bg=” av-desktop-hide=” av-medium-hide=” av-small-hide=” av-mini-hide=” av-medium-font-size-title=” av-small-font-size-title=” av-mini-font-size-title=” av-medium-font-size=” av-small-font-size=” av-mini-font-size=”][/av_heading]
[av_hr class=’invisible’ height=’25’ shadow=’no-shadow’ position=’center’ custom_border=’av-border-thin’ custom_width=’50px’ custom_border_color=” custom_margin_top=’30px’ custom_margin_bottom=’30px’ icon_select=’yes’ custom_icon_color=” icon=’ue808′ font=’entypo-fontello’ admin_preview_bg=” av_uid=’av-h6nht’]
[av_textblock size=” av-medium-font-size=” av-small-font-size=” av-mini-font-size=” font_color=” color=” id=” custom_class=” av_uid=’av-7tsy9′ admin_preview_bg=”]
Ben Goss, MS and John Agee, MD.
Recently, we published a study that looked a bit closer at pressures in the carpal tunnels of 12 patients with idiopathic carpal tunnel syndrome (CTS) while they actively used their hands; “Dynamics of Intracarpal Tunnel Pressure in Patients With Carpal Tunnel Syndrome” (J Hand Surg 2010; 35A:197-206). While our research helped us better understand just how dynamic these pressures are during hand use, we questioned whether there might be more going on than we originally thought. Following are a few of the questions we pondered and our thoughts on what we think may be going on with these pressures in the carpal tunnel. If you’re interested in what we actually know, then please read our publication. If you’re curious about what we think may be going on, but don’t know for sure, continue reading. Maybe you’ll have some questions of your own.
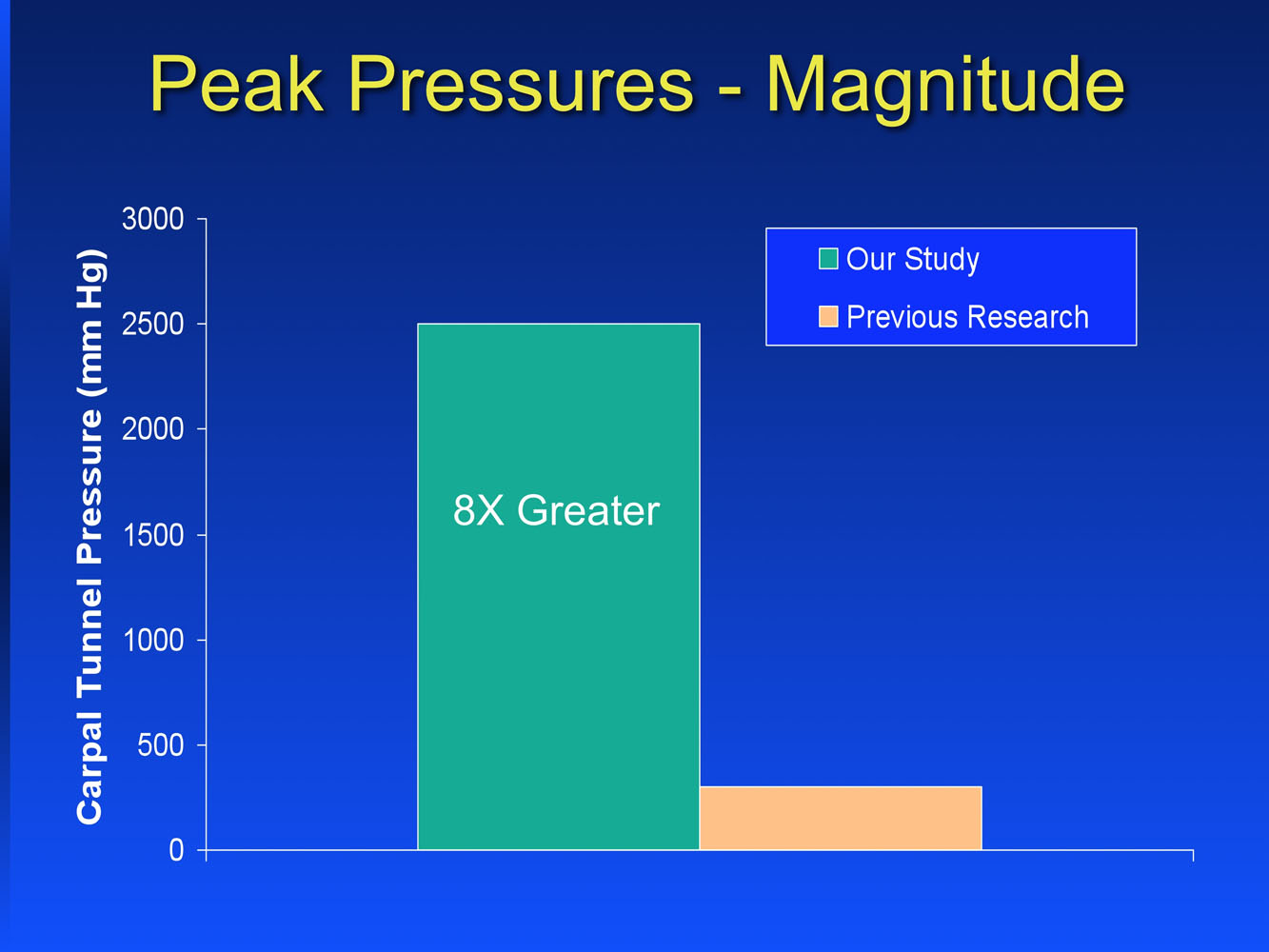
The highest pressures we recorded were about 8 times greater than what had been previously reported.
What could cause these higher than expected pressures?
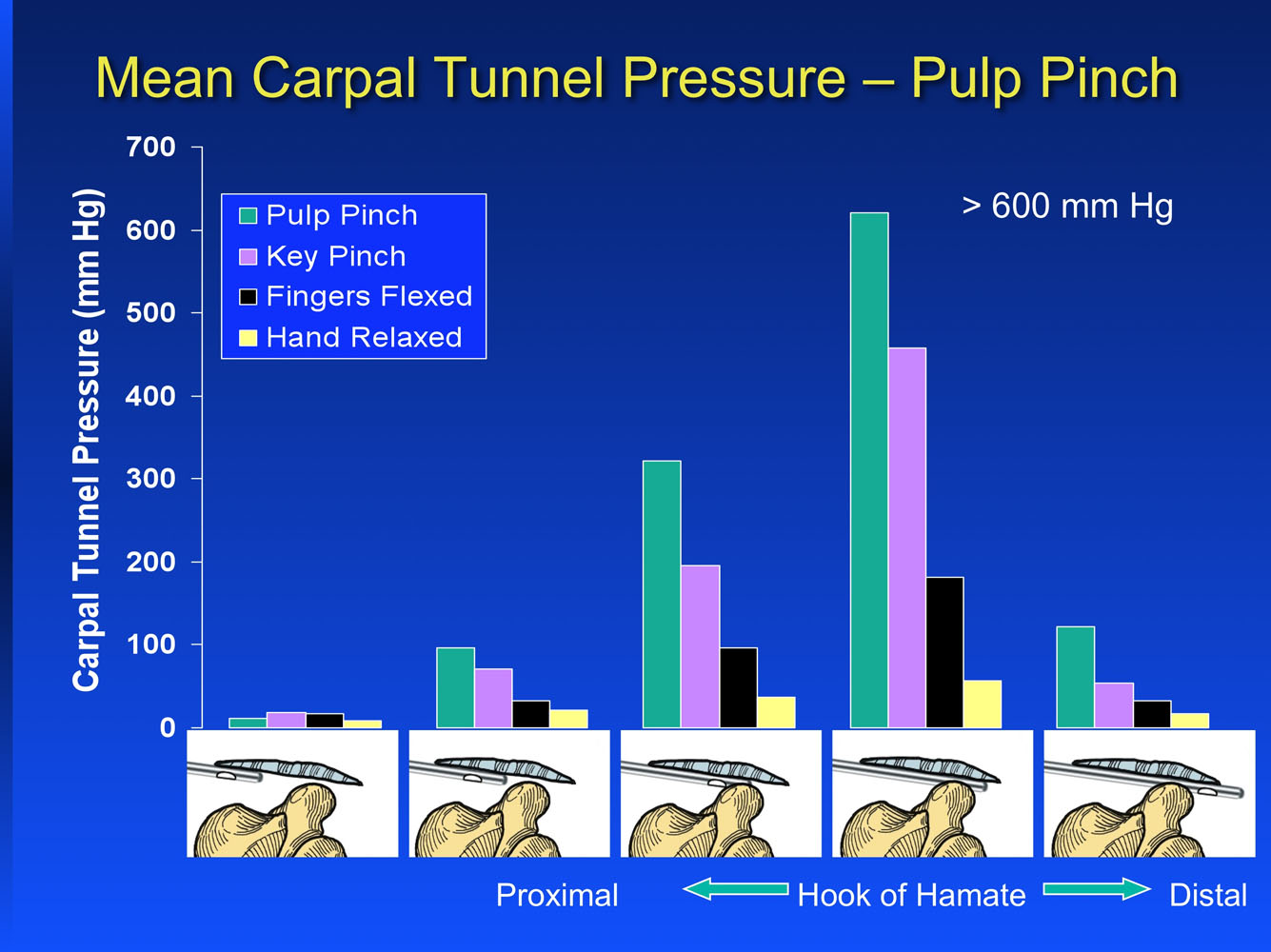
We believe that forceful contraction of the lumbrical muscles within the carpal tunnel may be the primary contributor. When any hand is used actively (like gripping a golf club or a hammer) and the fingers are flexed, the lumbrical muscles migrate proximally into the carpal tunnel. We saw a slight increase in pressure in the carpal tunnel when the patients just flexed their fingers, but this didn’t cause the really high pressures we recorded. The more forcefully patients used their hand (either gripping or pinching a dynamometer), the greater the pressure spiked. The highest pressures we measured were when the patients gripped a dynamometer with maximum force.
To get these maximum pressures, the fingers had to be flexed enough so that the lumbrical muscles moved proximally into the tightest part of the carpal tunnel and then the hand had to be used forcefully enough so the lumbricals contracted, “in synergy” with the finger flexor muscle-tendon units. When the lumbrical muscles move into the carpal tunnel, their additional volume raises the pressure some. But, it seems to be something else, like when the lumbricals actively contract and expand further, that causes the pressure to really soar. Only when the patients in our study, who were fully awake, used their hands forcefully by gripping a dynamometer in the operating room, did the pressures peak. When the patient’s hands were relaxed with their fingers extended and a force was applied to the palm of the hand, the pressures were only about half of what they were when the patients actively gripped with the same force.
Another contributor to these high pressures might be a change in the rigidity of the soft tissues that border and help constrain the contents of the carpal tunnel when the hand is used forcefully. When a hand goes from being relaxed to being used forcefully, the elastic ligaments and muscles that border the carpal tunnel tighten up. Part of the increase in stiffness occurs as the intrinsic and extrinsic muscles contract. Another part of the increase in stiffness is the hardness of the object being forcefully grasped by the hand. Both of these combined tend to cause a more rigid boundary for the contents of the carpal tunnel to come in contact with. Both a more rigid boundary and forceful hand use that causes proximal migration of the lumbricals into the tunnel and active contraction of the lumbricals while in the tight part of the carpal tunnel are how we like to think that these high carpal tunnel pressures are generated.
In our study, we didn’t report that we also measured carpal tunnel pressures in two subjects without CTS. We saw higher than expected pressures in those two subjects too, comparable with the patients with CTS. This led us to believe that the dynamic behavior of carpal tunnel pressure is not unique to patients with CTS. While we have data from only two subjects, we now believe that it occurs in everyone, and it happens for a reason.
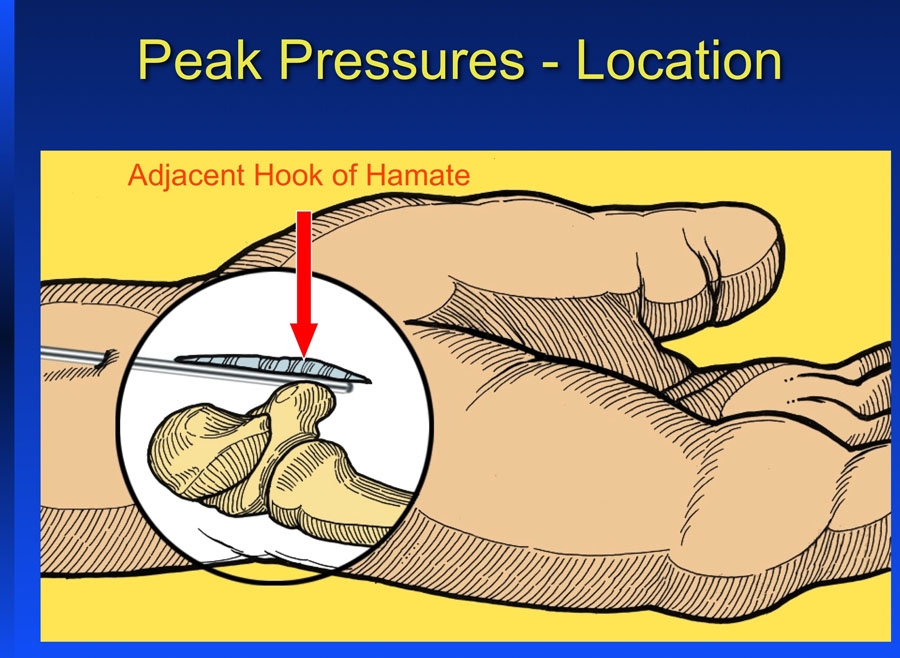
Previous studies did not identify that the maximum pressure occurs adjacent the hook of the hamate. Why was this consistently the location of maximum pressure in every subject we tested?
This may be a combination of the pressure sensor we used, the position of the pressure sensor within the tunnel, and the structural anatomy of the carpal tunnel. In our study, we used a pressure sensor that measured both hydrostatic pressure (like the pressure you feel when you’re underwater) and contact pressure (like the pressure you feel against the palm of your hand when you hold something). Then we positioned that pressure sensor between the contents of the carpal tunnel (flexor tendons, median nerve, synovium, lumbrical muscles) and the dorsal surface of the flexor retinaculum. When the hand was relaxed, the pressure sensor measured the resting hydrostatic pressure. When the hand was active (pinching and gripping dynamometers) the sensor was pressed against the dorsal surface of the flexor retinaculum as the lumbrical muscles pistoned from distal to proximal, into and out of the carpal tunnel. By being sandwiched between the contents of the carpal tunnel and the flexor retinaculum, our pressure sensor measured the dynamic behavior of the contact pressure as the hand was used.
The type pressure sensor and its positioning weren’t the only reasons. The pressure sensor had to be in the correct proximal-to-distal location. The transverse carpal ligament (TCL) is the segment of the flexor retinaculum that attaches to the pisiform, hook of the hamate, tuberosity of the scaphoid, and ridge of the trapezium. Because of its structural attachments, it is the stiffest segment of the flexor retinaculum. Because the TCL provides the real restraining force that stops the contents of the carpal tunnel from moving in a palmar direction, it makes sense that the greatest contact pressure…and therefore greatest ischemia producing compression on the median nerve…would occur where the ligament is the most stiff.
Based on the combination of the type pressure sensor we used, its location between the contents of the carpal tunnel and the dorsal surface of the TCL, and the anatomic configuration of the flexor retinaculum, it made sense to us that the maximum pressure would occur adjacent the hook of the hamate. Peak pressure adjacent the hook of the hamate also correlates with where the constricted part of the median nerve is found in patients with CTS, squeezing the life’s blood out of the patient’s precious median nerve.
The combination of these higher than expected pressures and their concentration along the stiff part of the TCL may not be coincidental. Could there be some functional significance to this dynamic behavior of carpal tunnel pressure?
Remember, this is only what we think. Our research didn’t actually produce any direct evidence that these dynamic pressures, those that cycle up and down as we use our hands, play a functional role. In fact, a lot of the previous research might lead you to conclude that doing anything that increases pressure in the carpal tunnel might contribute to CTS. But, a closer look at the research shows that it’s only an increase in the resting, or hydrostatic, carpal tunnel pressure beyond a threshold (most accept 30 mm Hg as the threshold) that contributes to CTS. The role of these dynamic pressures, those that occur during active hand use, remains unknown. We think that there may be a purpose for these dynamic pressures. So, we proposed a new theory to help explain one possibility for these dynamic pressures in the etiology of CTS.
We propose that these higher than ever before seen pressures may actually be normal and needed on a regular basis. Think of the pressure in the carpal tunnel as acting like a balloon trying to expand against the anatomic boundaries of the carpal tunnel. The structures that form these boundaries are the carpal bones and ligaments, with the TCL being the most obvious. These structures may need a regular dose of some serious stress to maintain the optimum shape and size of the carpal tunnel. Providing this stress may be the functional role of these dynamic pressures. There have been a few clues in the literature that relate to our theory.
First, the TCL has certain mechanical properties (i.e. its strength and stiffness) that are partially determined by both the size and number of collagen fibrils that it’s made of. In patients with CTS, both the size and number of collagen fibrils in the TCL are different than the fibrils in subjects without CTS. This alteration in mechanical properties may be a factor in the etiology of CTS [1]. Second, myofibroblasts have been found in the TCL’s of patients with CTS, suggesting that the TCL may be constantly trying to shorten [2]. Third, using hand exercises to create stress in the TCL has been promoted as necessary to maintain its length and reduce the signs and symptoms of CTS [3,4]. These findings all help support our idea that the fibrils of the TCL may be changing their morphology because of a lack of regular and sufficient mechanical stress.
This shouldn’t be any surprise; ligaments all over the body try to shorten if they are not regularly stressed. The same occurs with the TCL. If there’s not enough regular mechanical stress, the TCL starts to shorten. It transitions from being just the right compliance to be both a competent pulley and permit adequate perfusion of the median nerve to being this rigid constraint. If the TCL becomes too constraining, the contents of the carpal tunnel can’t expand as they need to, causing the resting pressure to creep up. If the TCL isn’t being stressed enough, it may be because it’s not getting enough cycles of this increased pressure.
So, how do you get the pressure in the carpal tunnel high enough and regularly enough to stress the TCL, preserve its elastic properties, and resist contraction? Using your hands forcefully. As we discussed above, forceful hand use delivers the lumbrical muscles into the carpal tunnel and then, with their active contraction, releases a cyclic force that acts against the TCL to dilate the tunnel. This may be the key to achieving the level of stress that the TCL needs, as well as the other ligaments that form the structural boundary of the carpal tunnel. It may be a completely normal physiologic function that one day we will accept that it’s only when the hand is doing real work that you can reach these stress levels. So, does a sedentary hand contribute to the onset of CTS? We’re not sure, but we do believe there is something significant about the dynamic behavior of carpal tunnel pressures that, if better understood, might help us better understand not only CTS, but also other symptoms that often present clinically along with CTS, such as trigger finger.
We hope you enjoyed our thoughts and if you have any constructive criticism, we would appreciate hearing from you.
References:
1. Stransky G, Wenger E, Dimitrov L. Collagen dysplasia in idiopathic carpal tunnel syndrome. Path Res Pract 1989;185:795-798.
2. Allampallam K, Chakraborty J, Bose K, Robinson J. Explant culture, immunofluorescence and electron-microscopic study of flexor retinaculum in carpal tunnel syndrome. J Occup Environ Med 1996;38:264-271.
3. Sucher B. Myofascial manipulative release of carpal tunnel syndrome: documentation with magnetic resonance imaging. JAOA 1993;93:1273-1278.
4. Sucher B. Palpatory diagnosis and manipulative management of carpal tunnel syndrome. JAOA 1994;94:647-663.
[/av_textblock]